To communicate with platelets and start the process of cancer spread, ovarian cancer cells are able to break the barriers of blood vessels and let platelets inside the tumor environment, according to a study that used microfluidic organ-in-a-chip technology.
Atorvastatin, a medication belonging to cholesterol-lowering statins, is able to maintain blood vessel integrity and prevent this interaction between cancer cells and platelets, potentially preventing cancer growth.
The study, “OvCa-Chip microsystem recreates vascular endothelium–mediated platelet extravasation in ovarian cancer,” was published in the journal Blood Advances.
Interactions between cancer cells and platelets help drive metastasis of ovarian cancer, the process by which cancer spreads to other parts of the body.
However, it was not previously known how ovarian cancer came into contact with platelets, prompting a team of researchers from Texas A&M University and the University of Texas MD Anderson Cancer Center to investigate this phenomenon.
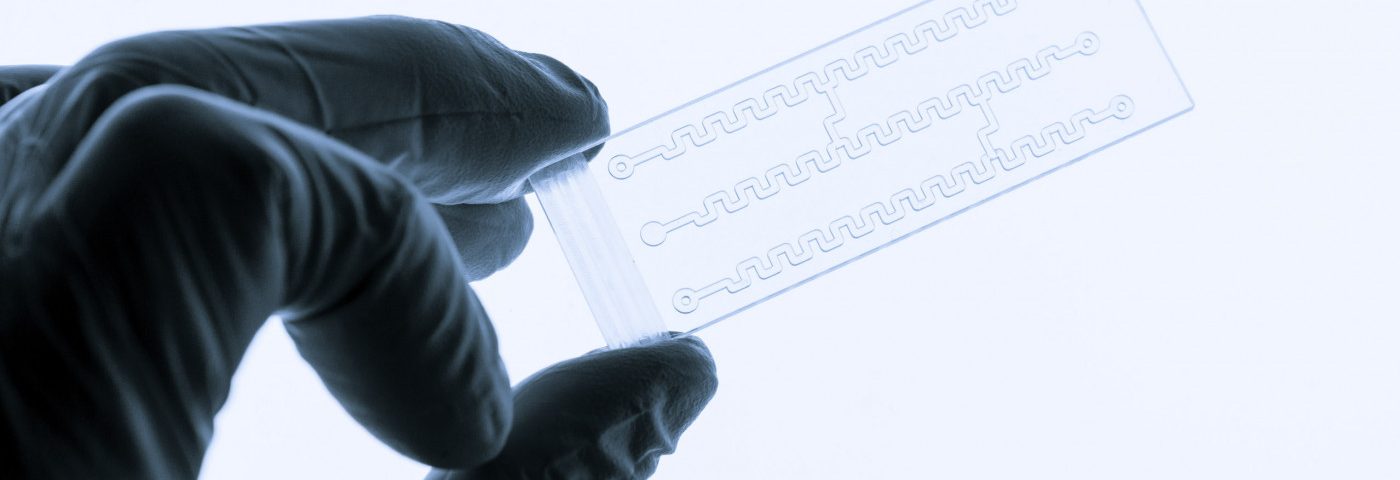
To model the relationship between ovarian cancer cells and blood cells, the research team used a device called an OvCa-Chip developed by Texas A&M researchers.
The three-dimensional device, roughly the size of a USB flash drive, can model the structure of a blood vessel. It contains living cells as part of its design, and has microfluidic properties to allow for the flow of fluids throughout the system, mimicking blood vessels.
The technology is termed organ-on-a-chip, as the device is designed to mimic the structure of an organ system on a smaller scale.
In the study, researchers lined the OvCa-Chip with endothelial cells, the type that make up the walls of blood vessels, and allowed them to grow for 24 hours. Afterwards, a small population of ovarian cancer cells was inserted in a small region of the chip.
The goal was to evaluate how the ovarian cancer cells interacted with the local endothelial cells, to better understand this dynamic and design treatments in the future that might take advantage of this improved understanding.
“It basically is a microenvironment where ovarian tumor cells can be co-cultured along with their blood vessels, and then they can interact with blood cells,” Abhishek Jain, MD, assistant professor at Texas A&M, said in an interview with the International Society on Thrombosis and Haemostasis, according to a university press release. “Once we learn about these interactions, we can then move forward to look into how drugs will impact these kinds of interactions.”
After 48 hours of co-culturing the blood and ovarian cancer cells, the researchers found a few gaps in the blood vessel structures, but throughout the next five days, they observed progressive breakdown of the vessel wall structure.
These findings were confirmed not only visually, but by the decrease in expression of a protein called VE-cadherin, an adhesion molecule that is involved in maintaining the integrity of blood vessel walls.
To further model the cellular dynamics, the researchers then introduced platelets into the OvCa-Chip system 48 hours after the co-culture.
The study found that the platelets exhibited similar behaviors that occur during the progression of ovarian cancer. The platelets were activated, moved towards the surface of cancer-influenced blood endothelial cells, and ultimately entered into the tumor environment.
Statins are cholesterol-lowering drugs that have also been seen to improve the outcomes of ovarian cancer patients. These medications are known to preserve blood vessel integrity, but whether outcomes of these cancer patients are improved through that mechanism is unknown.
To explore that, researchers treated the co-culture with atorvastatin. As expected, this significantly improved blood vessel integrity and reduced platelet activation, preventing the interaction between platelets and ovarian cancer cells.
“Therefore, our data predict that statins potentially serve as drugs that prevent cancer growth, partially by arresting their direct contact with platelets,” the researchers wrote.
Finally, they validated their findings in ovarian cancer biopsies from patients who had been treated with atorvastatin and those who had not. Again, patients on atorvastatin had significantly lower amounts of platelets inside their tumors, confirming the potential of this treatment approach.
Overall, this study not only confirmed the relationship between platelets and ovarian cancer, but also that the OvCa-Chip model could adequately be used as a model for blood vessel structures and for responses to treatment.
The researchers believe that the OvCa-Chip technology has the potential to be used for personalized medicine, as stem cells collected from a patient could be used to generate all of the blood cells used in the chip.
“So what we think the future for this technology is, is perhaps we can advance it in the direction of personalized medicine where we could actually take stem cells from patients and other patient-derived cells and make this entire chip from a single patient,” said Jain.