Researchers at Northwestern University have identified and mapped the location of structural proteins within pig’s ovaries, which closely resemble human ovaries.
This will help the development of an ovary-specific bio-ink that can be used to three-dimensionally (3-D) print artificial, implantable human ovaries that will allow infertile women to bear children.
“This is a huge step forward for girls who undergo fertility-damaging cancer treatments,” Monica Laronda, PhD, the study’s senior author, said in a press release.
“Our goal is to use the ovarian structural proteins to engineer a biological scaffold capable of supporting a bank of potential eggs and hormone producing cells. Once implanted, the artificial ovary would respond to natural cues for ovulation, enabling pregnancy,” she said.
The study, “Proteomic analyses of decellularized porcine ovaries identified new matrisome proteins and spatial differences across and within ovarian compartments,” was published in the journal Scientific Reports.
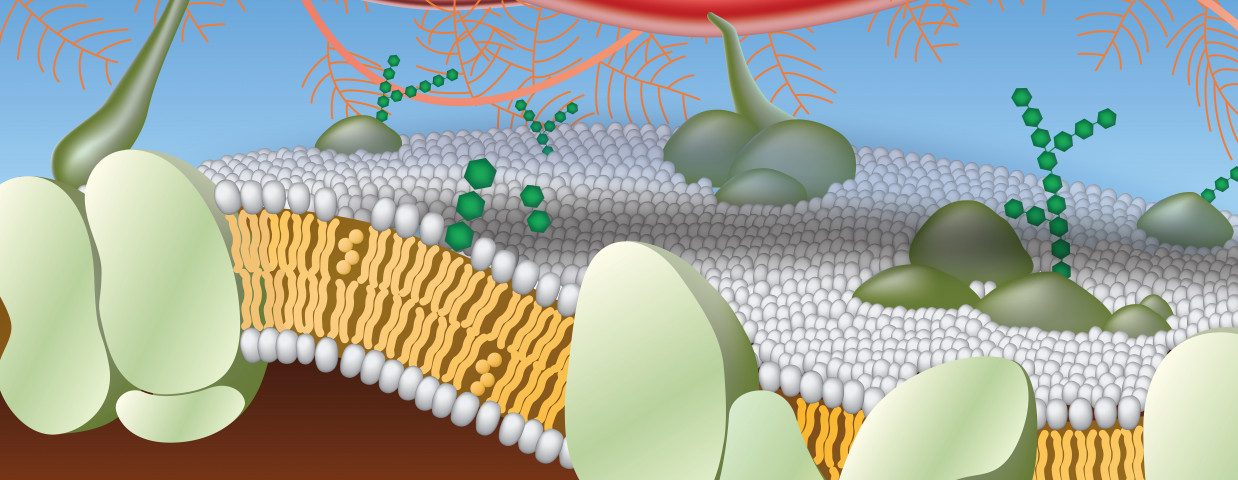
Cells of all tissues and organs are surrounded and supported by the extracellular matrix (ECM), a complex 3-D network of structural proteins and other molecules. This network provides not only a physical scaffold, but also several biochemical signals that regulate cell function.
Bio-ink is the material used in 3-D molecular scaffolds to produce engineered live tissue using 3-D printing technology. This scaffold supports the survival and function of its introduced cells, and the formation of blood vessels that will allow a healthy nutrient flow and communication within the organ and with the whole body.
All tissues and organs have a specific combination of ECM and ECM-associated proteins — called the matrisome — and a specific structure and organization. Thus, an organ-specific bio-ink must respect several chemical, physical, and biological constraints to develop a functional organ.
The ovary is divided into two visibly distinct compartments: the external, denser cortex, containing the reserve of follicles — fluid-filled structures in which the egg matures — and the internal medulla, containing most of the activated and growing follicles.
Laronda and her colleagues in 2017 showed that implanting a 3-D printed artificial ovary into a sterile mouse restored its fertility, with the mouse giving birth to a healthy litter. The researchers used a 3-D printed scaffold — based on a collagen-derived bio-ink — populated with ovarian follicles. Collagen is the ECM’s main protein component.
In November 2019, Laronda and three other collaborators received a patent for the creation of an artificial human ovary. The team’s goal is to help restore fertility and hormone production in women who have undergone cancer treatments at any point in their lives, resulting in an increased risk of infertility and hormone-based developmental issues.
The researchers’ first step was to determine the ovarian cortical and medullary matrisome signatures by identifying and mapping structural proteins in the two main ovarian compartments.
The project required comprehensive examination of the matrisome of pig ovaries, “as they have similar compartmentalization and [follicle developmental] waves to human ovaries and can be processed in the same way,” the researchers said.
“The structural proteins from a pig ovary are the same type of proteins found in humans, giving us an abundant source for a more complex bio-ink for 3-D printing an ovary for human use,” said Laronda.
Their innovative analysis methods allowed the identification of 42 structural proteins that were present at significantly different levels across ovarian depths, and 11 structural proteins that have not been reported in previous ovarian protein studies.
“These data have provided novel insights into matrisome quantity and compartmentalization and experiments that reveal the roles of matrisome proteins in controlling [follicle development] were selected from this analysis and are ongoing,” the researchers said.
“We are one step closer to restoring fertility and hormone production in young women who survive childhood cancer but enter early menopause as a late effect. There are still several steps to go and we are excited to test our new inks,” Laronda added.
Notably, the team’s methodology for identifying and mapping ovarian structural proteins also can be used to investigate, and potentially 3-D print, other organs of interest.
“We have developed a pipeline for identifying and mapping scaffold proteins at the organ level. It is the first time that this has been accomplished and we hope it will spur further research into the microenvironment of other organs,” Laronda said.
Laronda also serves as the director of basic and translational research, fertility & hormone preservation & restoration program at the Ann & Robert H. Lurie Children’s Hospital of Chicago. She is an assistant professor of pediatrics at Northwestern University Feinberg School of Medicine.