The levels of certain white blood cells in tumors correlate with longer overall survival in patients with some types of epithelial ovarian cancer, regardless of first-line chemotherapy or the extent of residual disease, researchers have found.
The study, “Dose-Response Association of CD8+ Tumor-Infiltrating Lymphocytes and Survival Time in High-Grade Serous Ovarian Cancer,” was published in the journal JAMA Oncology.
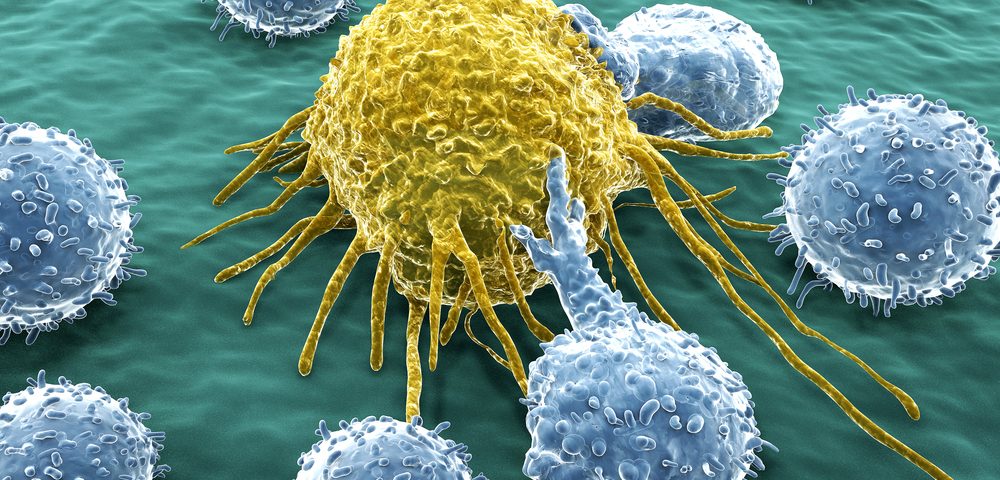
A subset of white blood cell, known as CD8-positive tumor-infiltrating lymphocytes (TILs), can kill tumor cells after being activated by degraded proteins. Previous studies have shown that CD8-positive TILs are associated with a better prognosis for patients with epithelial ovarian cancer. Researchers from the Ovarian Tumor Tissue Analysis (OTA) Consortium aimed to clarify the details of this association.
In the study, the levels of CD8-positive TILs were assessed in 5,577 patients with primary epithelial ovarian, peritoneal, or fallopia
n tube cancer, including 3,196 with high-grade serous ovarian carcinomas (HGSOCs). The mean age at diagnosis was 58.4 years.
The study showed an association between longer survival and increasing levels of CD8-positive TILs in HGSOCs. Indeed, while the median survival for patients with negative CD8-positive TILs was 2.8 years, those with high levels of these cells lived for a median of 5.1 years. This represented a 43 percent reduction in the risk of death, compared those with no detectable levels of CD8-positive TILs.
A similar trend was also observed in patients with endometrioid and mucinous ovarian cancer, but not in patients with clear cell ovarian cancer and low-grade serous ovarian cancer. This was the first study addressing the role of CD8-positive TILs in histotypes other then HGSOC.
Interestingly, TIL levels were also linked to survival in patients with BRCA1 mutations and non-carriers, but not in patients with BRCA2 mutations.
The authors conclude that “these large-scale analyses show that CD8+ TILs vary by histotype with HGSOC tumors having the highest levels and a strong association with survival, regardless of extent of residual disease or first-line chemotherapy treatment.”
Furthermore, “the extent of infiltration is prognostic, not merely its presence or absence, [suggesting] that understanding factors that drive infiltration will be the key to unraveling outcome heterogeneity in this cancer.”
Based on these results, a “clinically applicable scoring system” for CD8-positive TILs should be developed to be used in clinical trials, the researchers wrote.