A research team at the University of Wisconsin-Madison, led by professor of biomedical engineering and medical physics Paul Campagnola, is using innovative 3-D printing approaches to develop tools for imaging and detecting ovarian cancer. They aim to enhance scientific and medical understanding of how ovarian cancer cells develop and interact with nearby body tissue.
A research team at the University of Wisconsin-Madison, led by professor of biomedical engineering and medical physics Paul Campagnola, is using innovative 3-D printing approaches to develop tools for imaging and detecting ovarian cancer. They aim to enhance scientific and medical understanding of how ovarian cancer cells develop and interact with nearby body tissue.
Funded with a $2 million grant from the National Institutes of Health, the scientists are using technology they developed at UW-Madison to capture tissue images from surgical patients. The first target is collagen, a protein that holds bones, ligaments, and muscles together.
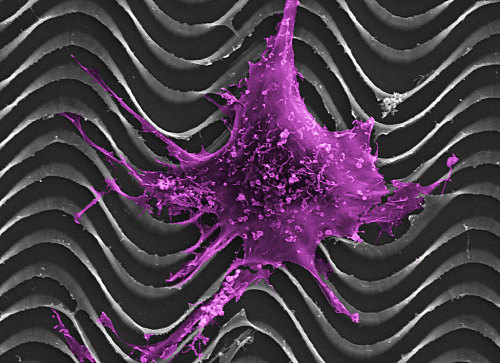 A normal ovarian epithelial cell clings to a tiny model of an ovarian cancer tumor made with a 3-D printer. The tumor models will help scientists study ovarian cancer in mice, which do not naturally develop the disease. Image courtesy of Paul Campagnola
A normal ovarian epithelial cell clings to a tiny model of an ovarian cancer tumor made with a 3-D printer. The tumor models will help scientists study ovarian cancer in mice, which do not naturally develop the disease. Image courtesy of Paul Campagnola
“In most cancers, including ovarian, there are large changes in the collagen structure that goes along with the disease,” Campagnola said in a UW-Madison press release. “It might happen first. It might be later. It’s actually not known.”
 Campagnola and colleagues hope to eliminate that unknown by printing tiny, 3-D models of the collagen samples.
Campagnola and colleagues hope to eliminate that unknown by printing tiny, 3-D models of the collagen samples.
Colleagues include Kevin Eliceiri, director of UW- Madison’s Laboratory for Optical and Computational Instrumentation (LOCI) — a biophotonic instrumentation lab that develops new techniques for imaging living things; UW-
Madison’s Laboratory for Optical and Computational Instrumentation (LOCI) — a biophotonic instrumentation lab that develops new techniques for imaging living things; UW- Madison associate professor of obstetrics and gynecology Manish Patankar; medical physics
Madison associate professor of obstetrics and gynecology Manish Patankar; medical physics  professor Tim Hall; and biomedics engineering assistant professorJeremy Rogers. The team is working under National Science Foundation
professor Tim Hall; and biomedics engineering assistant professorJeremy Rogers. The team is working under National Science Foundation  Major Research Instrumentation funding and the Morgridge Multiscale Initative. They seek to develop multimodal instrumentation to capture images of collagen so that cells and tissue can be measured in nanometers to centimeters, which will help better understand the role of collagen organization in cancer.
Major Research Instrumentation funding and the Morgridge Multiscale Initative. They seek to develop multimodal instrumentation to capture images of collagen so that cells and tissue can be measured in nanometers to centimeters, which will help better understand the role of collagen organization in cancer.
The UW-Madison scientists’ models will be biomimetic (synthetic, but mimicking biological materials) and extremely small in order to allow the researchers to implant the models into mice, after seeding them with ovarian cancer cells
The painstaking imaging and 3-D printing process for injecting mice with ovarian cancer is necessary because mice do noty get ovarian cancer — which partly accounts for why the cancer is not as understood as other cancers.
“The current way that people study ovarian cancer in a mouse is very poor,” Campagnola said. “They just take human cell lines and then inject them into a mouse. Then some of them will form into a tumor, but most do not.”
He hopes that implanting a 3-D tissue model seeded with ovarian cancer into mice will more closely mimic metastatic ovarian cancer development in humans.
“What’s different is our tissues will already be 3-D structured,” Campagnola said in the UW-Madison release. “One problem when people study cancer sometimes is that they put cells in a dish. Cells in a dish don’t act like cells in tissue. So we’re trying to give them the tissue structure that cancer cells would have in a native environment.”
The UW-Madison scientists will study how the implanted tumors grow inside the mice; learn more about the cues and processes involved in ovarian cancer’s development, progression, and spread; and improve imaging techniques for ovaries inside the body.
“It’s an integrated approach to improving our imaging capabilities, but then also using our imaging capabilities to make these models so we can study the biology,” Campagnola said.
According to the Mayo Clinic many women with ovarian cancer are not diagnosed until late in the disease’s progression, after the cancer spreads within the pelvis and abdomen and becomes late stage cancer, which is more difficult to treat and frequently fatal. Early-stage ovarian cancer, in which the disease is confined to the ovary, is more likely to be treated successfully.
The 5-year relative survival for all types of ovarian cancer is 45%, according to The American Cancer Society (ASC), but women diagnosed when they are younger than 65 do better than older women — and if ovarian cancer is treated before the cancer has spread outside the ovary, the 5-year relative survival rate is 92%. But only 15% of all ovarian cancers are found at this early stage.
The UW-Madison research team’s long-term goal is to improve screening, diagnosis and treatment of ovarian cancer by developing a straightforward method for screening women with higher risk for developing the disease, and improving the outlook for those who do. For example, women who carry a mutation of the BRCA gene implicated in higher breast cancer risk, leading some to prophylactic mastectomies, also have a 40 percent chance of developing ovarian cancer.
“Those are the women we really want to follow,” Campagnola said. “You could imagine — we’re a long way off from this — screening those women every few years with a minimally invasive device through a laparoscope or through the fallopian tubes.’
But researchers need to know a lot more about how ovarian cancer works first.
“You have to know what you’re looking for,” Campagnola said. “That’s why we have all this more basic work to do to get to that point. That’s why we need better imaging tools and we need better models to understand the biology of the disease.”